If you’re evaluating EHR software development, treat it as a clinical workflow + regulatory + interoperability program, not “just another SaaS build.” Most failures come from (1) unclear clinical workflows, (2) under-scoped integrations, (3) weak data governance, (4) usability debt, and (5) compliance handled too late.
What I’d do in your position:
1) Map 3–5 highest-impact workflows end-to-end, 2) agree on a minimum interoperable data set (FHIR resources + vocabularies), 3) define a security/compliance baseline early (HIPAA/GDPR/PDPA/APPs), 4) run a thin-slice prototype through real clinicians, and 5) choose build vs buy using a total cost of ownership (TCO) model.
Key takeaways
-
EHR vs EMR: EHR is designed for broader interoperability and continuity of care; EMR is often more “within one organization.” (Vendors vary, so define it in your requirements.)
-
Interoperability is not optional: Build around HL7 FHIR and plan for SMART on FHIR if you need app extensibility and modern authorization patterns.
-
Compliance is design input, not a checklist: HIPAA Security Rule expects administrative/physical/technical safeguards; NIST provides practical guidance to implement them.
-
Usability drives adoption and safety: Poor UI increases documentation time, workarounds, and clinician burnout. Budget for user research and usability testing.
-
Build vs buy is usually “hybrid”: Many organizations buy a certified core and build differentiating workflows, patient portals, and analytics on top via APIs.
Introduction: Why EHR Software Development Matters Today
What EHR software is (plain definition): An Electronic Health Record (EHR) system is software that stores, manages, and exchanges patient health information to support clinical care, operations, compliance, and reporting across a healthcare organization, and increasingly, across organizations.
Why custom EHR development differs from off-the-shelf: Off-the-shelf EHRs optimize for broad market fit and compliance; EHR software development for a specific organization optimizes for your workflows, integrations, and strategic differentiation. That’s valuable, but it also transfers more responsibility to you (security, regulatory compliance, uptime, and change management).
Who this guide is for:
-
Healthcare providers modernizing legacy systems
-
Digital health startups building vertical EHRs
-
Enterprises integrating EHR/EMR modules into platforms
-
Procurement teams comparing vendors vs custom builds
What you’ll learn:
How EHR development and EMR software development decisions affect cost, timelines, clinical efficiency, interoperability, risk, and long-term operational flexibility, plus a practical process, stack guidance, and a decision checklist (useful when working with EMR software developers or an EHR software development company).
What Is EHR Software? (Foundational Understanding)
EHR vs EMR (define once, then be consistent)
-
EMR (Electronic Medical Record): commonly refers to a digital version of a patient chart within a single practice/organization.
-
EHR (Electronic Health Record): commonly implies broader sharing and interoperability (labs, imaging, pharmacies, other providers), with stronger emphasis on continuity of care.
In practice, vendors use the terms loosely, so in EMR development and EHR software development, define scope by use cases and interoperability requirements, not marketing labels.
Core purpose of EHR systems
A modern EHR supports:
-
Clinical care delivery (documentation, orders, results, e-prescribing, clinical decision support)
-
Operational efficiency (scheduling, revenue cycle management, utilization reporting)
-
Regulatory compliance (privacy, audit trails, retention, breach handling)
-
Interoperability (exchanging data using standards like HL7 FHIR)
How EHRs support workflows
EHRs sit at the center of:
-
Clinical workflows: triage → encounter → orders → results → follow-up
-
Administrative workflows: registration → eligibility → billing → claims
-
Regulatory workflows: access controls, audit trails, breach notification processes
Common misconceptions (that derail projects)
-
“We can bolt interoperability on later.” Usually false; data models and integration architecture patterns should be designed early.
-
“Clinicians will adapt.” They will—by creating workarounds that harm data quality and safety.
-
“Compliance is a final QA step.” Compliance requirements shape architecture, logging, encryption, and access control from day one.
How EHR Software Improves Clinical Workflows (with Practical Examples and Pitfalls)
This is where EHR software development creates measurable value—when it removes friction from high-volume workflows.
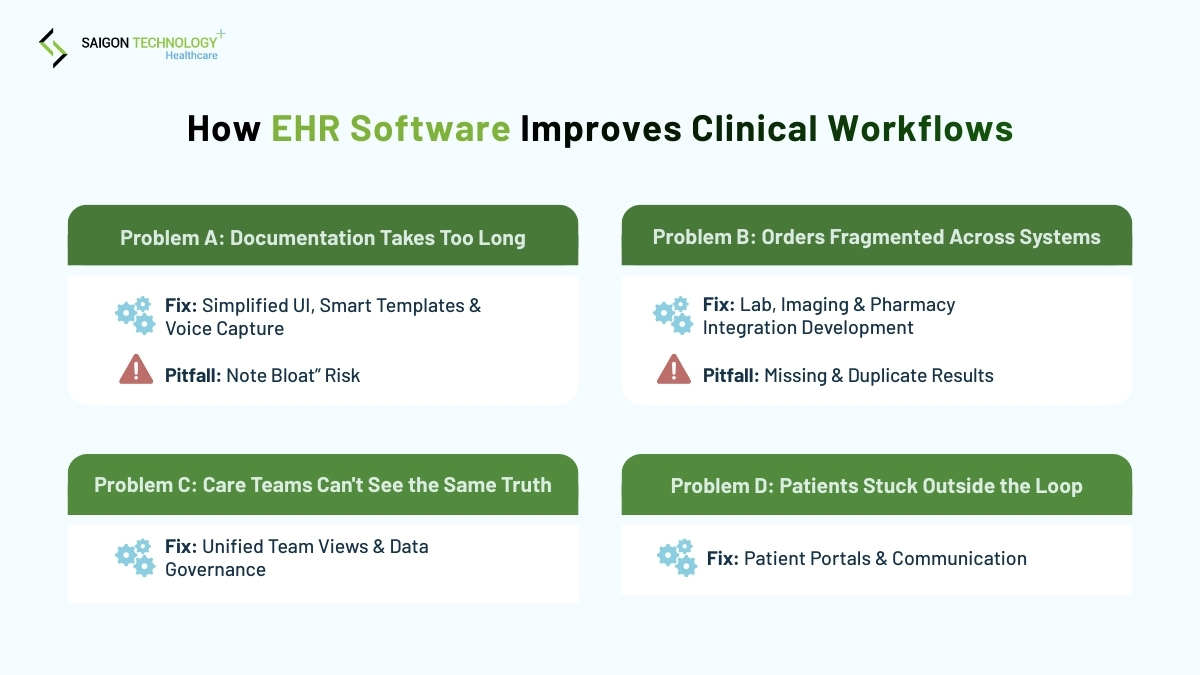
The clinical workflow problems EHRs can solve (and how)
Problem A: Documentation takes too long
-
Fix: reduce user interface complexity, use templates intelligently, automate structured data capture, and integrate voice recognition carefully (with review workflow).
-
Pitfall: over-templating creates “note bloat” and can increase medical error risk.
Problem B: Orders/results are fragmented across systems
-
Fix: integration development with labs/imaging/pharmacy, unified inbox/tasking, and status tracking.
-
Pitfall: “best-effort” interfaces without reconciliation logic create missing results and duplicate orders.
Problem C: Care teams can’t see the same truth
-
Fix: role-based, team-based views; consistent patient identity; problem list governance; data ownership rules.
Problem D: Patients are stuck outside the loop
-
Fix: patient portals, patient management portal features (appointments, results, messaging), and clear consent flows to improve patient satisfaction.
Practical “thin-slice” example (what I’d do)
If you’re unsure where to start with EMR software development, pick one end-to-end “thin slice,” such as:
New patient intake → visit note → lab order → result review → patient message → billing handoff
Build/prototype this slice first. It forces stakeholder requirements gathering, integration requirements, and security requirements into one contained scope before you scale.
Key Features of a Modern EHR System
Below are the core features most decision-makers expect in EHR software development companies’ proposals. Use these as a requirements baseline, then add your unique workflows.
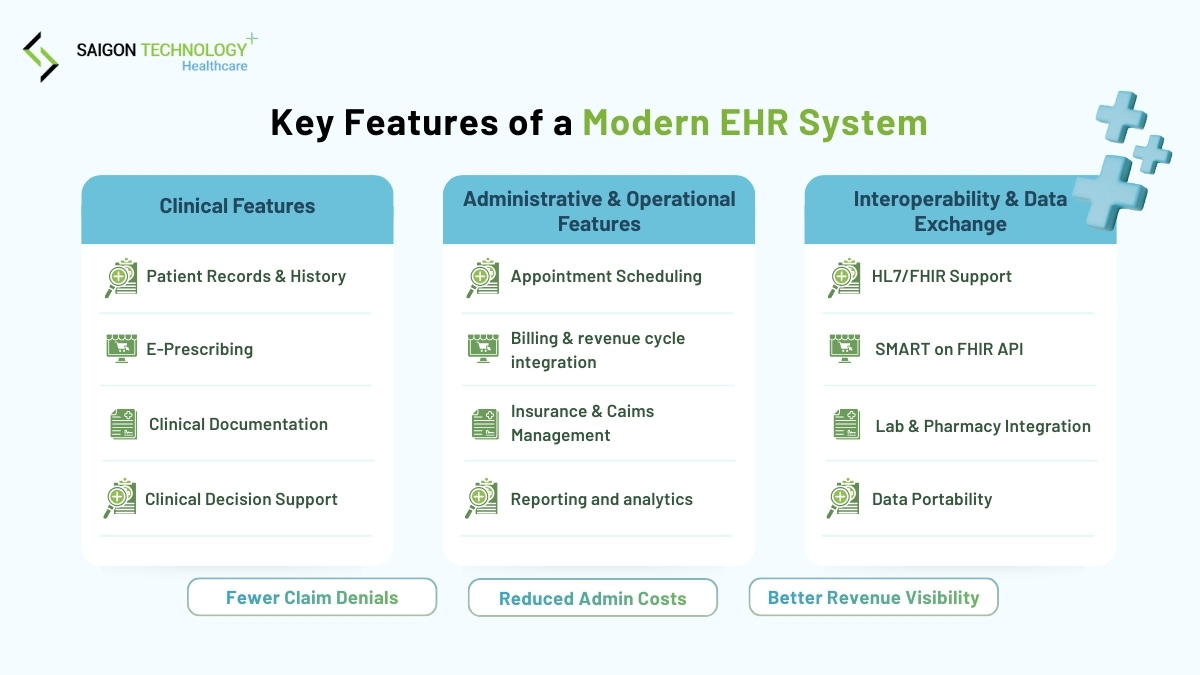
1. Clinical features
-
Patient records & medical history: problems, meds, allergies, immunizations, encounters
-
Clinical documentation & charting: notes, structured forms, templates, attachments
-
E-prescribing: medication selection, safety checks, refill workflows (country-specific)
-
Clinical decision support (CDS): alerts, reminders, guideline prompts, risk scores (with careful governance)
Regulatory note (US): CDS can intersect with FDA oversight depending on functionality and intended use; understand how your CDS features are categorized.
2. Administrative & operational features
-
Appointment scheduling: multi-location, provider templates, reminders
-
Billing & revenue cycle integration: coding support, claim generation, payment posting, denial workflows
-
Insurance and claims management: eligibility checks and payer interfaces vary by region
-
Reporting and analytics: quality reporting, operational efficiency dashboards, throughput
Where you often see real ROI:
-
Billing accuracy improvements (fewer denials, cleaner claims)
-
Administrative cost savings through automated eligibility, reduced rework
-
Better revenue cycle management visibility (aging, denial reasons)
3. Interoperability & data exchange
Interoperability should be explicit in your EHR development scope:
-
HL7 / FHIR support: FHIR is a widely used API-focused standard for exchanging healthcare information.
-
SMART on FHIR: adds a secure app integration layer using open standards like OAuth2 and OpenID Connect.
-
Integration with labs, imaging, pharmacies, and devices: plan for interface monitoring, retries, reconciliation, and downtime behavior
-
Data portability: export and patient access patterns; consider Bulk Data where relevant (population health, analytics)
Common challenges in EHR software development (and how to mitigate)
These are the failure modes I see most in EHR software development and EMR software development programs.
1. Clinician adoption and resistance to change
Mitigation: clinician champions, shadowing, iterative usability testing, phased rollout, and clear “what changed” training.
2. Poor usability leading to burnout
Mitigation: user research + wireframing + usability testing as first-class deliverables. Track “time to complete” for key tasks and reduce clicks.
3. Integration with legacy systems
Mitigation: invest early in integration architecture patterns, interface observability, and a canonical data model. Budget for “unknown unknowns” in legacy systems.
4. Regulatory changes and long approval cycles
Mitigation: regulatory compliance planning and compliance testing integrated into each release, not end-loaded. Use security implementation process checklists.
Compliance, Security, and Privacy Requirements
This section matters for business decision-makers because compliance failures become financial risk, reputational risk, and downtime risk.
1. U.S. compliance (HIPAA)
The HIPAA Security Rule requires “reasonable and appropriate” administrative, physical, and technical safeguards for protecting ePHI.
A practical implementation guide is NIST SP 800-66 Rev. 2, which maps security program activities to HIPAA requirements.
What to build into your EHR from day one:
-
Access controls (role-based access controls, least privilege)
-
Audit trails (who accessed what, when, from where, what changed)
-
Data encryption (at rest and in transit)
-
Breach notification procedures readiness (logs, incident response playbooks)
2. Global & regional considerations (EU, Singapore, AU)
-
EU (GDPR): health data is treated as a special category; you need a valid legal basis/condition and strong safeguards.
-
Singapore (PDPA): PDPA sets obligations for collection, use, disclosure, and care of personal data; PDPC provides healthcare sector guidance, including transfer limitation and breach notification obligations.
-
Australia (APPs): the Australian Privacy Principles are the cornerstone framework under the Privacy Act 1988, governing how covered entities handle personal information (including health information guidance).
Practical guidance: If you operate across regions, design around the strictest common controls: data minimization, explicit access control, auditability, retention policies, and cross-border transfer controls.
3. Security best practices (applied, not abstract)
For EHR software development company evaluations, ask whether they can operationalize these:
-
RBAC + MFA (multi-factor authentication): enforce MFA for privileged access; review roles quarterly
-
Segmentation of environments: separate prod/non-prod; never use real patient data in test unless you have a formal process
-
Threat modeling and secure SDLC: require code review, dependency scanning, and penetration testing
-
Security verification standard: OWASP ASVS provides a concrete checklist of web application security controls and test requirements.
-
Disaster recovery: define RPO/RTO targets and run restore tests (not just backups)
Interoperability Standards and Data Governance
Why interoperability affects outcomes and cost
Interoperability reduces duplicate testing, supports continuity of care, and enables safer coordination, but only if data quality and governance are enforced.
The standards you should know (simple explanations)
-
HL7 FHIR: standard for exchanging healthcare information electronically, optimized for modern APIs.
-
SMART on FHIR: a standards-based way to let third-party apps securely integrate with EHRs using OAuth2/OpenID Connect.
-
HL7 CDA: document markup standard for clinical documents exchange (still relevant in many ecosystems).
Real-world use cases for FHIR-based APIs
-
Patient-facing apps accessing records (with proper consent)
-
Provider-to-provider exchange and referral workflows
-
Population health management and predictive analytics pipelines
-
Device and IoT device integration (where appropriate governance exists)
Data governance (the “unsexy” part that saves projects)
Define:
-
Data ownership: who owns problem list, meds, allergies, demographics
-
Data quality rules: required fields, code systems, validation checks
-
Access control model: data access control by role, location, encounter, and sensitivity
-
Retention and deletion: align with regulatory requirements by region
Avoiding vendor lock-in:
Lock-in often happens at the data model + integration layer. The best defense is:
1) enforce API-first patterns (FHIR where feasible), 2) maintain an internal canonical model for analytics, and 3) ensure you can export data in a usable format.
Custom EHR Development vs Ready-Made Solutions
This is where most executive teams need decision support.
1. When custom EHR development makes sense
Custom EHR software development is usually justified when you have:
-
Specialized clinical workflows (e.g., oncology protocols, complex multi-disciplinary pathways)
-
Differentiation needs (unique patient experience, proprietary care models)
-
Integration complexity (many legacy systems + custom processes)
-
A long runway where operational flexibility matters more than speed
2. Pros and cons comparison (build vs buy vs hybrid)
| Option | Best for | Strengths | Trade-offs/risks |
| Buy a ready-made EHR/EMR | Standard workflows, faster go-live | Known feature set, vendor support, sometimes certification-ready | Customization limits, licensing fees, integration constraints, vendor roadmap risk |
| Build custom (full) | Unique workflows, platform differentiation | Full control, tailored UX, flexible integrations | Higher implementation risk, longer timelines, must own compliance/security and ongoing operational costs |
| Hybrid (common) | Most mid-to-large orgs | Buy core + build modules (patient portal, analytics, specialty workflows) | Requires strong integration architecture patterns and governance to avoid “two EHRs” experience |
What I’d do in your position:
If you’re in the US and need regulatory alignment with certified ecosystems, I’d seriously consider a hybrid approach and validate interoperability requirements early (FHIR + SMART where relevant). For US programs that interact with certified EHR technology, note how the Promoting Interoperability programs emphasize interoperability and use of certified EHR tech.
Ideal Technology Stack for EHR Software Development
There’s no single “best” stack, but there are predictable requirements: auditability, security, scalability, integration performance metrics, and maintainability.
A practical reference architecture
- Frontend: modern framework (React/Angular/Vue) with strict accessibility and component governance
- Backend: modular services (not necessarily microservices on day one), strong domain boundaries
- Database systems: relational core for transactional integrity; consider separate analytics store
- Search: for chart search and document retrieval (with strict access controls)
- Integration layer: API gateway + message/eventing where needed; interface engine for HL7 v2 where relevant
- Identity & access: MFA, RBAC, and audit logging centralized
- Cloud infrastructure: choose a cloud platform selection based on regional hosting, compliance, and vendor support; hybrid approaches if required
Stack selection criteria (what procurement should ask)
- Can you support system downtime gracefully (read-only mode?, queued orders?)
- How do you isolate tenants and sensitive workflows?
- How do you handle data migration and data validation at scale?
- What is your approach to testing and quality assurance, including security and usability testing?
- What’s the plan for annual maintenance and support costs?
EHR Software Development Process (Step-by-Step)
This process applies whether you’re working with an EHR developer team in-house or outsourcing to EMR software developers.
1. Discovery & requirements analysis
Do stakeholder requirements gathering with:
- Clinicians (different specialties, nurses, allied health)
- Admin staff (front desk, billing, medical records)
- IT/security/compliance
- Finance/procurement (cost constraints, vendor requirements)
Deliverables that reduce risk:
- Workflow maps (current vs future)
- Market research and feasibility analysis (what must be integrated, what can change)
- Data governance decisions and regulatory compliance planning
2. UX/UI design for clinicians
Non-negotiables:
- User research: shadowing, contextual inquiry
- Wireframing + prototyping: test with real scenarios
- Usability testing: measure task completion time and error rates
- Accessibility and responsive design (clinics, wards, tablets)
3. Architecture & technology decisions
Decide early:
- Cloud vs on-premise vs hybrid (data residency, latency, operational maturity)
- Integration architecture patterns (sync vs async, retries, idempotency)
- Scalability planning (peak hours, batch jobs, reporting)
4. Development & testing
A healthcare-appropriate QA strategy includes:
- Functional tests for critical flows (meds, allergies, orders)
- Security testing (penetration, dependency, config)
- Performance testing (peak clinic hour)
- Compliance testing (audit trails, access controls)
- Validation and UAT with clinicians (realistic scripts)
5. Deployment & maintenance
Plan for:
- Deployment planning and preparation (cutover checklists, rollback plans)
- Go live support and monitoring (war rooms, incident triage)
- Data migration (reconciliation reports, clinician sign-off)
- Ongoing updates with documented change management
Best Practices for Successful EHR Development (and cost/timeline reality)
Best practices
- Clinician-first design (optimize for clinical efficiency, not admin convenience)
- Incremental rollout with feedback loops
- Observability built-in (integration monitoring, audit trails, uptime metrics)
- Security requirements embedded from sprint 1 (HIPAA/GDPR/PDPA/APPs)
- Strong documentation and training to support user adoption and training
Cost and timeline expectations (how to think about it)
Instead of guessing a number, use a simple ROI calculation framework and a cost breakdown:
- Cost components: engineering, QA experts, compliance testing, infrastructure costs, third-party integrations, licensing fees (if hybrid), training
- Hidden costs: integration requirements growth, data cleansing for migration, downtime contingencies, security audits, support staffing
- Ongoing operational costs: monitoring, patching, incident response, annual maintenance and support costs
What I’d do in your position:
Build a business case development doc with:
- Top 3 operational pain points (measurable)
- Target improvements (billing accuracy, reduced rework, faster throughput)
- Implementation risks and mitigations
- TCO over 3–5 years (build vs buy vs hybrid)
Decision checklist (use this in procurement and executive reviews)
Strategy & scope
1. What’s our non-negotiable scope (must-have workflows) vs phase 2?
2. Are we building EHR, EMR, or a hybrid around existing systems?
Compliance & risk
3. Which regulations apply (HIPAA, GDPR, PDPA, APPs) and where will data be stored?
4. Do we have defined access control, audit trails, encryption, and breach processes?
Interoperability
5. Which integrations are required at go-live (labs, imaging, pharmacy, payers)?
6. Are we using HL7 FHIR and do we need SMART on FHIR app integration?
Usability & adoption
7. Have clinicians validated prototypes with realistic scenarios?
8. Do we have a training and change management plan?
Operational readiness
9. What are uptime targets, RPO/RTO, and downtime procedures?
10. Do we have monitoring, incident response, and support staffing?
Future trends in EHR software development (what’s real vs what’s hype)
AI-assisted clinical documentation (real, but governance-heavy)
Generative AI can reduce documentation burden, but you must design for:
- clinician review/attestation
- traceability (what was suggested vs accepted)
- data privacy and model boundaries
Predictive analytics and population health management
Value depends on data quality, coding consistency, and governance; otherwise, you get false signals.
Patient-centric, interoperable ecosystems
FHIR + SMART patterns continue to expand app ecosystems and patient access models.
Regulatory evolution (especially around CDS)
In the US, the FDA provides guidance clarifying which CDS functions may be excluded from device definition and which may remain regulated, which is important if your EHR includes advanced CDS or patient-facing decision logic.
Conclusion
EHR software development works best when you treat it as a clinical workflow and risk-management program, not a typical software build. The highest-impact teams start by mapping a few high-volume workflows, validating them with clinicians, and designing interoperability (HL7 FHIR), security, and auditability from day one.
Whether you choose custom build, a ready-made platform, or a hybrid approach, the real differentiators are usability, integration reliability, data governance, and a realistic total cost of ownership (TCO) model that includes support and compliance. If you focus on measurable outcomes, clinical efficiency, billing accuracy, and patient satisfaction, you’ll invest in an EHR that strengthens operations instead of creating long-term complexity.
Contact Saigon Technology for an EHR software development consultation. With 14 years of experience, proven delivery across the US, Australia, Europe, and Singapore, and practical AI integration for healthcare, we’re ready to help. Let’s discuss your roadmap.
FAQ
1. What’s the difference between EHR software development and EMR software development?
In practice, they overlap. EMR software development often focuses on internal charting and practice workflows, while EHR software development more often emphasizes interoperability and continuity of care. Define the difference in your requirements, not by vendor terminology.
2. How long does EHR software development take?
For a meaningful first release, many teams need 6–12 months, depending on integrations, data migration, and compliance scope. Full replacement programs can take longer. The biggest drivers are integration complexity and stakeholder requirements gathering.
3. What standards should our EHR support?
At a minimum, plan for HL7 FHIR for modern API interoperability. If you need third-party apps to launch inside the EHR securely, consider SMART on FHIR.
4. What compliance requirements matter most across the US, EU, AU, and Singapore?
- US: HIPAA Security Rule safeguards (admin/physical/technical).
- EU: GDPR, including stricter handling of health data.
- Singapore: PDPA obligations and PDPC healthcare guidance, including transfer limitation and breach notification.
- Australia: APPs and health privacy guidance.
5. How do we estimate the total cost of ownership (TCO)?
Include:
- build cost (engineering + QA + product + security)
- integration development and interface monitoring
- infrastructure + environments
- compliance audits and security testing
- training, go-live support, ongoing maintenance
Then compare build vs buy vs hybrid over 3–5 years.
6. How do we choose between an EHR software development company and building in-house?
If speed and compliance maturity are concerns, an experienced EHR software development company can reduce delivery risk—but only if you retain ownership of requirements, governance, and clinical validation. In-house teams offer tighter control long term but require a strong security/compliance operating model.
7. What should we ask EMR software developers in an RFP?
Ask about:
- prior healthcare integrations (HL7 v2, FHIR, imaging, labs)
- security implementation process (MFA, RBAC, encryption, audit trails)
- usability testing approach with clinicians
- downtime procedures and monitoring
- experience with multi-region regulatory requirements
8. Does clinical decision support make our EHR a regulated medical device in the US?
Not always. FDA guidance clarifies how certain CDS functions may be excluded from device definition and when FDA oversight may apply, this depends on the function and intended use. Get regulatory counsel if you’re building advanced CDS.
Author (experience & perspective)
Phuc (Cris) Tran – Author: Healthcare Software Development Consultant specializing in EHR/EMR platforms, interoperability, and security by design.
How this guide was written: Based on common delivery patterns and risks seen across EHR modernization programs, aligned to publicly available regulatory and standards references cited above.
Sources (selected)
- HHS: Summary of the HIPAA Security Rule
- NIST: SP 800-66 Rev. 2 (HIPAA Security Rule implementation guidance)
- HL7: FHIR Overview
- SMART Health IT: SMART on FHIR API overview
- EU GDPR: Article 9 (special category data, including health data)
- Singapore PDPC: PDPA overview + Healthcare sector advisory guidelines
- OAIC (Australia): Australian Privacy Principles + health privacy guide
- FDA: Clinical Decision Support Software guidance